COVID Vaccine FAQs
You've had questions about COVID-19 vaccines, so we gathered our best answers from NFLPA Medical Director Dr. Thom Mayer as well as medical and scientific consultants Drs. Dan Hanfling and Peter Haaland.
Background on COVID and Immune Response
SARS Co-V-2 is a novel and emerging RNA virus from the coronavirus family, which means that it can only replicate (produce more virus) once it attaches to your cells, through a receptor site known as ACE-2.
The part of the virus which attaches to the ACE-2 receptor on the normal cells is known as the “spike protein,” which are the red “spikes’ on the virus’ surface (see below). This protein is responsible for the variants since it can change its structure over time, resulting in the South Africa, UK and Brazil variants of the disease.
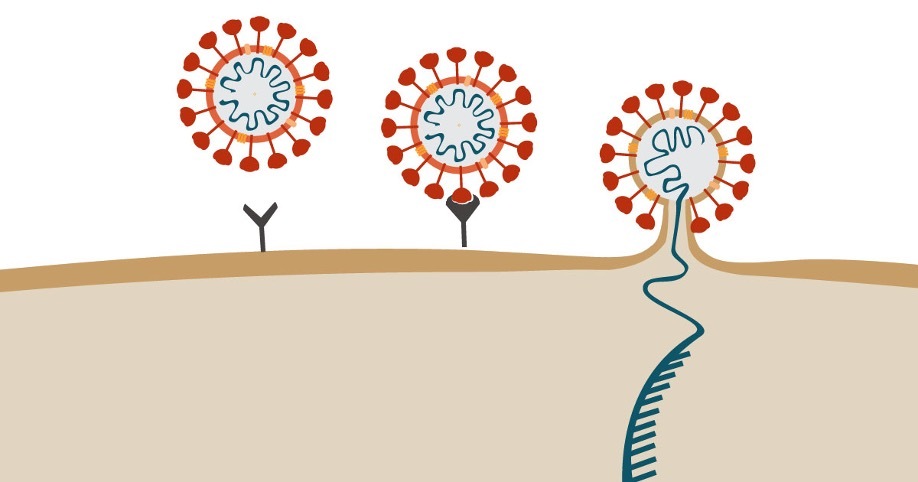
The spike protein is not the toxic part of the virus -- it is simply the “key” to unlock access to the cell, where the RNA itself is delivered and copies of the virus are made rapidly, as Figure 2 shows. This infects the cells, which then infect other cells in a cascade. Vaccines work by attaching to the spike protein and taking it out of circulation, thus preventing infection.
Originally, it appeared this was largely in respiratory cells, but as we better understand the virus, we now know that it also involves ACE-2 receptors in the vascular smooth muscle, which likely accounts for the highly inflammatory and multi-system aspects of COVID, as well as its long-term effects. It can also attach to the same receptors in cells in the gastrointestinal system, which explains why some patients with COVID have GI symptoms.
But for all we know and have learned in recent months, it remains unclear who might experience what symptoms; or why some people have symptoms ranging from mild to severe, while other patients are asymptomatic -- and yet remain capable of spreading the virus to others without knowing it.
A major part of the evolving fight against COVID is the utility and widespread use of vaccines since this virus has one natural enemy -- aerosolized or air-borne transmission. If we can shut off transmission, we can shut off the virus. The guidelines we used last year (testing, masking, physical distancing, etc.) were all designed to limit transmission. But the most reliable way to limit transmission of a virus is through effective vaccination – balanced, of course, with concerns about safety, effectiveness and efficacy, all of which we will discuss below and in detail.
Our bodies have an elegant, highly effective and fine-tuned -- but not perfect or foolproof -- way of detecting the presence of bacteria (living entities that can cause many infections, including pneumonia, soft-tissue infections, ear infections, urinary tract infections and many others) and viruses (non-living entities comprised of either DNA or RNA particles that can also cause infections, but rely on your own cells to multiply). The immune system’s role is to recognize these “invaders,” notice that “Wait, you’re not me; you shouldn’t be here!” and mobilize a response to clear the invader so it can’t cause any trouble.
While the immune system is complex, think of it as having two main “teams” -- each of which have a specific purpose -- that combine together to fight “intruders.”
B lymphocytes (a type of white blood cell-or WBC) - The primary role of B lymphocytes is to receive the signal that an intruder is present in the body and to make antibodies in the blood, which will attach to the intruder (also known as an “antigen”) and remove it from your system. Antibodies work immediately, can last for weeks to months, but may decline over time (which raises the potential need for “booster” vaccinations, which we will discuss below).
T lymphocytes (another type of WBC) - the T cells have many functions, but their main roles in this context are to fight already infected cells and act as the memory function of recognizing that the body has seen these intruders before and respond -- even if the circulating antibodies are gone or too low to deal with the challenge. They work from hours to days to months to years in the battle. For instance, the measles, mumps and rubella vaccines we all took as kids last for many years, largely through the memory T cell function.
Background on COVID Vaccines
The primary goal of vaccines is to use either a part of the virus or a placeholder that closely resembles the virus to induce an immune response -- including both antibodies (through B cells) and memory (through T cells). As a result, we will recognize the virus instantly and begin to remove it from our bodies before it can gain a toehold and produce a clinical infection and/or more copies of the virus.
In the context of COVID, there are two basic types of vaccines (among many, many types for other viruses): Messenger RNA (mRNA) vaccines and Viral Vector vaccines. They work with many similarities but some important differences. They both are intended to prevent transmission of the virus by significantly reducing the risk of contracting the virus; or, if we do end up catching the virus (because “breakthroughs” can occur, since no vaccine is 100% protective), it allows our immune system to fight off the infection more efficiently, reducing the likelihood of severe illness, hospitalization and death. Both types of vaccines have been shown to reduce all these outcomes dramatically.
As discussed above, RNA is not “alive” but carries a signal that can be thought of as holding the “key” to providing protein manufacturing instructions in the RNA. RNA works by getting into the area of the cell that is the “power plant” responsible for manufacturing whatever it is told. (The “power plants” are known as mitochondria. It is very important to know that the mitochondria do not have DNA in them, and the mRNA has no instructions to make DNA. Although DNA is in the nucleus, mRNA vaccines simply cannot make changes to your DNA or genetic makeup.)
The message that the mRNA sends is to make antibodies responsive to the part of the spike protein delivered via the vaccine. How do we know what the right directions are to make the antibody to the spike protein? Fortunately, early on in the course of this pandemic, scientists learned the specific gene sequence of the virus and its spike protein, so they created mRNA with the right instructions.
But we still have to get it to the right place and protect it during its journey. mRNA is easily degradable, even in the body, so it must be protected in order for it get into the cell and to the right place. That is where the beauty and utility of mRNA vaccines come into play. The technology of using this delivery vehicle has been conceived, evaluated and improved upon for well over 20 years (Note: This vehicle was championed and even developed by one of the NFLPA’s principal scientific advisors when he founded the Biotechnology Office (BTO) at DARPA, which is the Defense department’s area for innovative scientific developments). It was a highly attractive candidate for safely and effectively delivering instructions to the cell, well before the pandemic. (https://www.scientificamerican.com/article/genomic-vaccines/)
Now that we have instructions and a delivery mechanism to get this message to the cell, how do we protect the mRNA to assure it can get to the right place? Another stroke of genius was to package the mRNA in an encasement of harmless and easily degradable (once the message is delivered) layer of a lipid nanoparticle (think “oily shell”). This allows it to get into the cell, through the cytosol (cell matrix) and to the mitochondria. Therefore, the message is sent and delivered safely and harmlessly, using old technology for a new, innovative purpose. (The other requirement to keep the mRNA protected is lower storage temperatures, which have been easily attainable.)
The Pfizer and Moderna vaccines are both examples of mRNA vaccines. They have proven to be highly safe, effective and efficacious, with more than 200 million doses have been given. Several quick notes about the mRNA vaccines:
- They have been shown to be highly effective, resulting in high antibody levels in 92-95% of the people receiving it. (No vaccine is ever 100% effective). Even in the rare cases of fully vaccinated patients who still contract COVID (less than 0.01%), they still prevent severe forms of the disease that can lead to hospitalizations and death.
- They are also safe, with the trials in 30,000 and 40,000 patients (respectively) showing only minor side effects, including extremely rare severe allergic reactions (since there are no preservatives).
- They require two doses – the second of which should come 21-28 days after the first. While the body has a primary response to the first dose, the second dose results in a secondary response that is 100 to 1,000 times higher. This very likely means that the antibodies stay higher for longer, but we will only know for sure over time.
Viral vector vaccines use a modified version of a different virus (in this case, adenovirus) to deliver the same message to the cells. Johnson & Johnson (J&J) combined its efforts with another company, Janssen, to make these vaccines. Viral vector vaccines can use either weakened virus or inactivated virus to assure that the adenovirus carries the message to make antibody against the spike protein and warn the T cells to remember the spike protein. The J&J vaccine uses a human inactivated adenovirus as its delivery mechanism. (AstraZeneca, another company, makes its vaccines from chimpanzee adenovirus, but that is not used in this country).
The J&J vaccine, which is given in a single dose, was found to have a efficacy level of 65%. This means 65% of vaccinated people had sufficiently high antibody levels to prevent COVID infection. It is important to note that these trials occurred in South Africa, which had much higher rates of infection than the U.S., and during a time period when there were more COVID variants, which may account for some of the difference.
As you have undoubtedly read, a rare form of blood clotting known as cavernous venous sinus thrombosis (CVST) occurred with the J&J vaccine, which forced a “pause” in the use of the vaccine to study what was happening and why. The pause has since been lifted, and the incidence of CVST after vaccination was shown to be seven in one million, so it is rare. Importantly, the incidence of CVST in those with COVID is 40 in one million, meaning it is much riskier to experience this through COVID infection than through the J&J vaccine. All cases occurred in women ages 18-49, so the CDC does not recommend this vaccine for women in this age group.
As medical practitioners, we strongly encourage everyone and their families to become educated on the vaccines, how they work, and the positives and negatives of vaccination. To be clear, while I as your medical director, and the other experts consulted, encourage players to choose vaccination (and each of us made the choice to receive the vaccine early on), that is a personal decision only you and your family can make.
In the past, it was largely up to the various jurisdictions as to whether they had mRNA (Pfizer or Moderna) or adenovirus (viral vector/J&J) vaccines available. However, each day more and more supplies of all vaccines have become available and the goal is to assure that anyone over 16 can receive the vaccine (Note: On May 12, the CDC endorsed the Pfizer vaccine for children ages 12-15). As supplies continue to increase, it is likely many people will have the opportunity to choose which vaccine they get.
The quick, easy and accurate answer is “We don’t know yet.” (Remember this is a “novel and emerging” virus). Frankly, it is highly likely that booster vaccinations will prove to be the safest way to prevent the disease and its spread. But the entire scientific community (and the NFLPA’s expert advisers) will follow the science every day and go wherever it takes us.
There are two basic reasons why a booster may be needed. First, antibody titers may fall over time to a low-enough level that they need to be “boosted” back to a higher level. While that’s a possibility, the memory T cells we talked about will be very effective at seeing that spike protein again and will kick into high gear. Second, there are currently three primary variants of the virus (UK, Brazil and South Africa), all of which spread easily but none of which are more lethal than the main coronavirus. While the vaccines appear to be effective against all the variants, it may be necessary over time to have a booster that specifically addresses these variants. There is nothing unusual about this; viruses by nature make changes to their structure all the time. And there is very solid science emerging to indicate that the booster dose will be available in a nasal spray or pill.
COVID-19 Vaccine Questions
Two recent studies from Lancet and New England Journal of Medicine (NEJM) are testaments to the effectiveness and safety of the vaccines.
The Lancet article describes the experience in Israel, where 4.7 million (72%) of its population of 6.5 million are vaccinated:
- This is the first report of a nationwide COVID vaccination program.
- The Pfizer vaccine was greater than 94% effective against COVID infections, hospitalizations and deaths.
- The importance of a second dose was emphasized by the increased decline in death with two doses (96.7% decline) vs. a single dose (77% decline)
- 94.5% of the Israeli Covid infections were from the UK (B1.117) variant, indicating that even this mutation is protected by the Pfizer/mRNA vaccine
- During the study period, 50% of COVID cases were from the South Africa (B1.351) variant and 44.5% were caused by the UK variant (B1.117).
- 385,853 persons had one dose, while 265,410 had a second dose.
- The effectiveness against the South Africa variant was 75%.
- Effectiveness against the UK variant was 90%.
- Prevention against severe, critical or fatal disease was 97.4%
The NEJM article describes the experience in Qatar:
Similar studies will be compiled for the U.S. experience, but these two clearly indicate clearly that the mRNA vaccines are highly effective at preventing COVID infection and, to a greater extent, serious disease and death.
Extensive data show the vaccines trigger production of natural antibodies that inhibit growth of the virus in the body. They all work by exposing a person’s immune system to non-toxic fragments of the virus.
The mRNA vaccines (Pfizer and Moderna) enter muscle cells and signal them into producing various “spike” proteins, while the adenovirus viral vector vaccines (J&J and Astro-Zeneca/Oxford) introduce these fragments in an adenovirus (a common virus that causes mild irritation but no significant illness). There is a competition between rapid viral replication (exponential growth doubles the number of virus particles about every four hours) and viral removal by antibodies, B-cells and T-cells. If the immune response is too slow, it can be overwhelmed by virus and lead to severe disease or death.
Here are some other detailed reports:
In the U.S., scientists at every major research university and medical center are carefully compiling data and sending it to both the Centers for Disease Control and Prevention (CDC) in Atlanta and the National Institute for Allergy and Infectious Diseases (NIAID) in Washington, D.C. Studies from across the world are included in these analyses.
The basic biology of mRNA and adenovirus-based vaccines has been studied for decades and consensus has formed around the mechanisms behind triggering immunity in humans. The efficacy of each vaccine was initially measured by large-scale, double-blinded clinical trials in tens of thousands of volunteers. Half of these were given vaccine, and half were given an empty shot so that neither the volunteer nor the medical personnel who administered the dose knew whether they had real vaccine or a blank. The rate of infection of these groups was followed over months and the rate of infection (as measured by tests, reported symptoms, hospitalization, intensive care and death) were recorded. The vaccinated groups all showed lower numbers of infections, severity of disease and deaths compared with the ‘empty shot’ group.
Subsequent observations of much larger groups (hundreds of millions of persons) have confirmed the trial results that the likelihood of contracting the virus and the severity of an infection are both dramatically reduced by vaccination. However, the global population of virus is evolving in an environment of human immune responses in vaccinated and unvaccinated persons. It is likely (and has, in fact, been observed) that the current vaccines may be less effective to ‘evolved’ virus.
The table below shows the number of registered COVID-19 studies that are either vaccine related or have at least one drug intervention. The table also shows the number of "mapped drug names" retrieved by selected searches of COVID-19 studies.
Selected Search of ClinialTrials.gov1 | Studies | Vaccine Studies | Drug Studies | Mapped Drug Names |
All COVID-19 Studies | ||||
At least one U.S. location | ||||
U.S. Federal Funding |
The messenger RNA is enveloped in a layer of lipid (fat) that protects it from being destroyed by natural enzymes in our bodies. This fat is designed to have affinity for, stick to, and be ingested by normal cells. Once inside these cells, this RNA instructs the cell to manufacture fragments of the virus’ “spike” protein that is ultimately released and recognized by immune cells as an intruder. The immune cells respond by producing antibodies to this intruder so that when it is later identified on real virus particles, it tags the virus for destruction by the body’s immune system.
The varied responses to the vaccine, including efficacy and side effects, are due to the natural variability in the immune response portfolios of different individuals.
The mRNA is naturally destroyed by the body when it is unprotected by the lipid envelope. This is demonstrated with imaging studies at successive times with fluorescence labeled mRNA injected in mice.
The Pfizer and Moderna vaccines are the first mRNA vaccines to be approved for human use by the U.S. FDA. The mRNA method was developed more than three decades ago with applications in cancer and other diseases.
The mRNA does not interact with DNA, and it does not travel far from the site of injection. Within vaccinated cells, the RNA does not enter the cellular nucleus, which would be required for DNA interactions.
While we are not aware of “long-term” studies to test this hypothesis, there are no observations that indicate a cause-and-effect relationship between mRNA and DNA mutation.
Yes. And they are very safe since these types of lipids are routinely processed by the body without any side effects or negative consequences. The use of these lipid nanoparticles is a brilliant delivery mechanism to protect the mRNA message as it makes its way to the mitochondria.
There is no specific way to test if someone is allergic, but allergies are extremely rare. Further, these vaccines do not use preservatives and are not grown in egg culture, as many prior vaccines were. Allergy is one class of immune response, and an immune response is precisely why vaccines are used.
The relevant question is whether the immune response generated by the vaccine is harmful. Since every person’s immune system is different, among the hundreds of millions of doses that have been administered, very few immune responses have proven to be harmful. The research community is focused on identifying those cases.
For example, among approximately seven in one million women under 50, the J&J adenovirus vaccine is correlated with thrombolytic clots. Researchers are working to understand whether this correlation is causal and how to identify sub-populations that may be at risk for any harmful side effects.
The vaccines stimulate each individual’s immune system, and these differ among persons. They are most likely to be an enhancement of immunity rather than a detriment over the long term. However, the only sure answer to this question will come with continued observation of large and diverse populations. So far, there is no evidence of long-term detrimental effects.
All viruses mutate since that is a normal biological phenomenon. To date, the major variants of COVID are the UK, South Africa and Brazilian variants (the latter of which was responsible for the outbreak within the Vancouver NHL team). Each of these variants is more transmissible, but no more lethal than the original SARS-Co-V-2 virus.
Influenza virus is primarily transmitted by large droplets and intimate contact. SARS-CoV2 is primarily transmitted by small (~ 1 micron or .001 mm) aerosol particles that spread on air currents and are unknowingly inhaled. SARS is also more lethal than influenza, which is why it must be handled differently.
CDC epidemiologists have combined viral death information for many years. The incidence of influenza in 2020 has been dramatically reduced by the hygiene measures that were taken to combat COVID. SARS-CoV2 spreads more rapidly because of pre- and a-symptomatic transmission. It causes greater morbidity and mortality, and in some cases, leads to harmful lasting changes in individuals’ immune systems.
We don’t know precisely how many persons are asymptomatic and infectious. There is no clear answer to this question, other than that asymptomatic and pre-symptomatic transmission have been observed in various outbreaks and appear to be partly responsible for the pandemic. The R0 for SARS-CoV2, which is a measure of the rate of infection in an unvaccinated and immunologically naive population, ranges from 2 to 5, meaning it is highly transmissible. However, these estimates vary widely because the assumptions of the simplified models also vary among investigators.
The average diameter is about 85 nm (10-7 meters or 1/10,000 of a millimeter). If you laid 100,000 virus end-to-end in a line, they would span the width of your pinky fingernail.
These masks are designed to intercept 95% of salt aerosol particles 300 nanometers in diameter when the mask is sealed against the face. In fact, most masks leak around the periphery, so their effectiveness depends on how it’s worn and also the respiration rate of the wearer (since heavy breathing increases the pressure difference between inside and outside of the masks). The N-95 masks are fashioned from melt-blown polypropylene fibers that are electrostatically charged.
This varies widely depending on the thread count, fabric composition and the number of layers. This is a complex problem because filters that trap more particles also produce bigger pressure differences that increase leakage at the mask-face contact zones.
Virus particles don’t emerge as isolated fragments; they are encapsulated by fluid that includes water, protein, mucus and other materials. These moist aerosols are three times the diameter of the N95 salt aerosols and may be impeded by more porous masks, inhibiting transmission from and to a mask-wearer. Unfortunately, these aerosols may contain more than one virus particle, and since they emerge with very small diameter (~ 1/1000 of a millimeter), they do not settle to the ground. Instead, they remain suspended for hours and are transported by convection throughout an enclosed space.
There were 262 players and 464 staff with confirmed positive infections during the season, for an overall infection rate of nearly 3%. There was one hospitalization, but no ICU admissions or deaths reported. There were no cases of infection transmitted across the line of scrimmage.
Clusters of infection were clearly attributable to lapses in following protocols for mask use, social distancing and industrial hygiene. The protocols resulted in substantially lower infection rates among players and staff than in the surrounding populations.
Herd immunity is a theoretical, mathematical calculation to estimate what percent of the population would require immunity (either from vaccination or infection) to prevent transmission within a given population. It is based on simplistic assumptions regarding contact frequency, probability of transmission, duration of acquired immunity, lethality and a stable infectious threat.
Various models have predicted that this would occur between 70% and 80% immunity. As vividly illustrated by cases in Manaus, Brazil, these assumptions do not adequately describe the current pandemic. In Manaus, antibody measurements in the blood supply showed that 76% of the population had been exposed under conditions where ‘herd immunity’ was calculated to be 67%. Nevertheless, there was a massive outbreak because viral evolution produced variants that evaded human immunity.
While mathematical models can aid understanding of disease dynamics, including the impacts of vaccination and non-pharmaceutical interventions such as restrictions on congregate contact, mask use, ventilation and the like, the ‘herd immunity’ conversations in the media are mostly incomplete or misleading.
The simplified assumptions involved in herd immunity estimates are not satisfied in human populations with enormous variability in contact conditions, evolving virus and the discrete responses of varied immune systems.
Death rate is the number of deaths divided by the number of infections. Since vaccinated persons don’t get infected, they are not counted in either the numerator (number of deaths) or the denominator (number of infections) of this ratio, and therefore have no impact on it.
Hydroxychloroquine has been shown in clinical trials to be ineffective and reducing morbidity or mortality in COVID patients. While Remdesivir reduces the time to recovery for hospitalized patients from about 15 days to about 10 days, it has not shown any impact on less severe or asymptomatic cases.
A total of 1062 patients underwent randomization (with 541 assigned to Remdesivir and 521 to placebo). Those who received Remdesivir had a median recovery time of 10 days as compared with 15 days among those who received placebo.
Monoclonal antibodies (Regeneron) were used to treat former President Trump and other VIPs and have since shown effectiveness in reducing morbidity and mortality. It has been granted Emergency Use Authorization by the FDA.
No, this is extraordinarily unlikely since hundreds of millions of doses have been administered with nearly zero adverse effects and proven effectiveness.
The EUA is administrative; the challenge going forward will be to adapt our pharmaceutical and non-pharmaceutical responses including vaccines, therapies and behaviors more rapidly and effectively than the evolving virus.
Other Resources Discussing the COVID-19 Vaccine
WHOOP podcast (discusses vaccine effects viewed through resting heart rate, heart rate variability, sleep quality and quantity, and “recovery”)
Effect on COVID-19 vaccine on WHOOP data
Marshawn Lynch conversation with Dr. Fauci
COVID-19 vaccine and the Black community (Tyler Perry special)